- December 26, 2024
-
-
Loading

Loading
There have been numerous ways that medicine has been practiced throughout the centuries.
One of the first major approaches was home visits, where the town doctor would make personal visits to people with various ailments.
Then came the reverse, patients traveling to centralized hospitals and doctors for treatments. It’s been that way for some time, but a new approach is gaining prominence.
Telehealth — where a health care provider and patients communicate virtually in completely different physical spaces — has been an option for years but has seen a surge in popularity of late.
Part of that is necessity. The ongoing pandemic has caused hospitals and health providers to encourage as little contact as possible with contagious patients. But some medial professionals believe it’s now here to stay.
“I think it was inevitable that we're going to get to this point sooner rather than later,” said Michael Schandorf-Lartey, the chief medical officer at Doctors Hospital of Sarasota. “Obviously, the COVID-19 crisis basically created the existing situation. … [Telehealth] is not going to come down because it was headed there anyway.”
Here’s some information on what might be your next experience at a hospital.
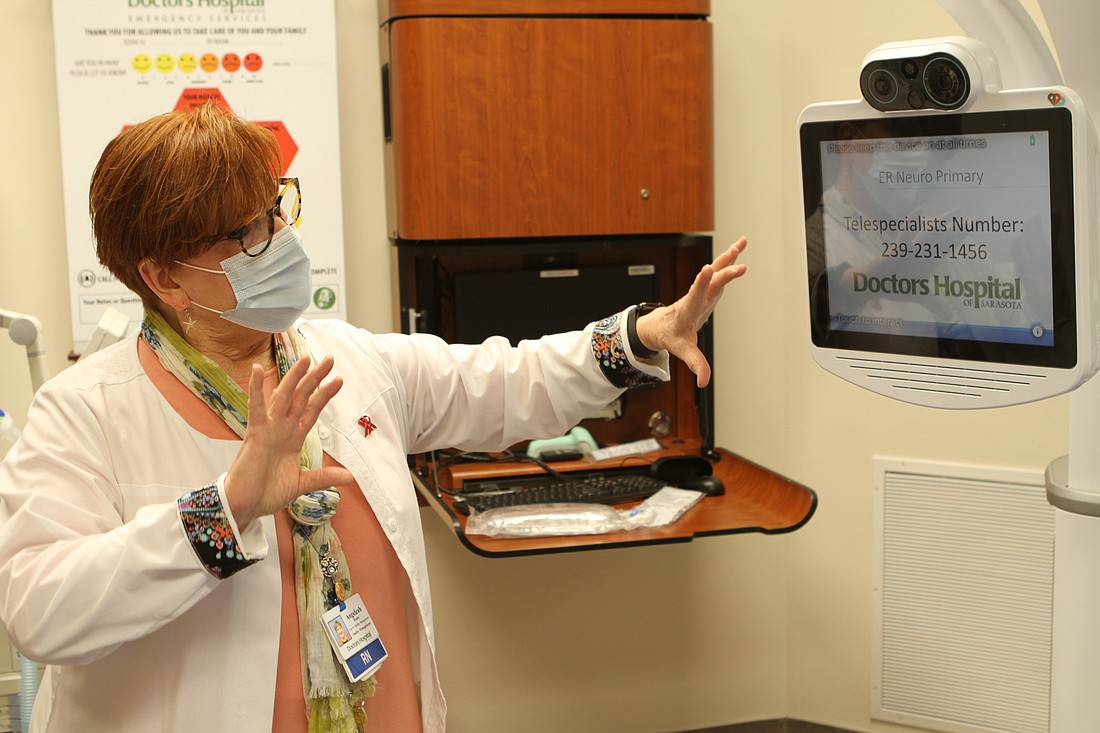
Health professionals use video telecommunication systems to treat patients remotely. This often involves video to get a better idea of what ails the patient. It can be done through iPads, iPhones and other forms of technology.
Telehealth allows health centers to connect with emergency physicians and specialists to consult and treat patients they wouldn’t be able to see otherwise. It also helps streamline and speed up taking care of patients, which can be critical in time-sensitive situations like having a stroke.
“We need to get them within the first three to four hours really with the onset of symptoms to be able to intervene and help them more acutely,” said Angeleah Halaby, stroke and sepsis coordinator for Doctors Hospital of Sarasota. “If it's an emergency, [and] you don't get here quick enough, then we can't give you the treatment that we need.”
A timely response from a health specialist working remotely can save time, which is valuable if the person’s brain is in danger.
Doctors Hospital of Sarasota started using the telehealth program with strokes last year.
The practice is more popular with the aforementioned stroke care, but it can also be seen in psychiatric treatment as well as with critical care patients in the intensive care unit. It’s particularly useful for professionals to determine whether a person needs temporary detainment at a treatment facility due to mental illness.
"You have this system where as soon as the patient comes in emergency room, or even before they come, you're activating the protocol," Schandorf-Lartey said. "So that psychiatrist is an online … and can assess the patient and can determine whether this is grounds for executing the Baker Act or sometimes that it doesn't exist and the patient can be treated. So it's very timely attention to the patient's needs and saves a lot of unnecessary Baker Acts."
In addition to emergencies, telehealth is commonly used for minor urgent care, such as seeing if a cut or bruise is serious or needing treatment for such ailments as pink eye or fever. It is also helpful for needing medication while you're out on vacation. Seasonal residents can rely on it to connect with a doctor no matter what home they're in, rather than having a doctor for both locations.
Most new technology takes a second to make sense, and family practice Dr. Meghan Buhler with First Physicians Group has recently implemented telehealth into treating her patients, many of whom are in their elder years. She says they’ve picked it up quickly.
"[My patients] access to us as a provider but didn't want to be near anyone," Buhler said. "It's been an adjustment, but everyone has been pleased with the outcome. My patients like being able to physically see me, and I like seeing them where we have that connection. … Even our patients who are older and might have had a negative thought about technology are surprisingly good at it. It's worked out really well."
Schandorf-Lartey said telehealth initially cost more than in-person meetings because of the cost of installing the video technology but has since evened out to the point that insurance companies cover more of the costs, so the price is comparable to an in-person meeting.
Florida does not currently require private payers to reimburse telehealth, but most large insurance carriers — including BCBS, Aetna, Cigna and United Healthcare — do cover it. The best way to know if your policy covers telehealth is to call your carrier directly and ask about eligibility.
The advantages of telehealth with its greater accessibility and efficiency are clear. The drawbacks, though, are harder to define. Schandorf-Lartey worries the transition to a digital approach will take something away — the human element of medicine.
“There's something to be said about sitting across someone and having them look into your face, talk to you about what's going on,” Schandorf-Lartey said. “But I think the downside is that we're going to lose something — that commonality, that feeling like we're all the same beings that are connecting on a certain type of level — we're going to lose that, and is it a justifiable loss? I think we might we might lose some of that, but I guess with any progressive system there are always positives and negatives, and this may be one of the negatives that we'll have to negotiate or navigate our way around.”