- November 13, 2025
-
-
Loading

Loading

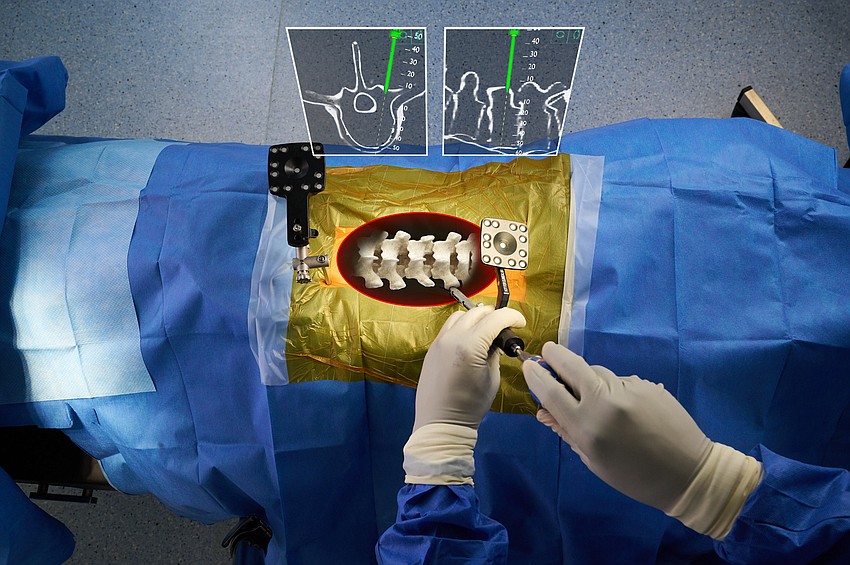
Sarasota Memorial Hospital recently deployed xvision, an augmented reality technology pioneered by Augmedics, which allows surgeons to literally see through skin and scar tissue to more accurately place rods and screws while reducing X-ray exposure, recovery time and complications that require return trips to the operating room.
The technology allows surgeons to perform complex procedures like spinal surgery without nearly as much cutting.
Designed as wearable technology that the surgeon can use while moving freely in the operating room, the xvision system is a headset with a high-speed processor and a transparent augmented reality display that the surgeon looks through while operating.

With a CT scan providing the necessary anatomic data, the xvision headgear can project a detailed 3D model of the patient’s spinal structure onto the surgeon’s display in real time.
A built-in tracking system ensures the 3D model perfectly aligns with the patient’s true anatomy, so when surgeons look down at the patient, it’s as if they are looking through tissue directly to bone — and from every angle — without the encumbrance of wires or bulky equipment.
Dr. Lam Nguyen, an orthopedic surgeon at Kennedy White Orthopedic Center in Sarasota, has employed the xvision technology at SMH for nearly six months. He has yet to have a patient return to the operating room for a surgical revision, he said.
“Because we relied on traditional 2D X-ray guidance, there is always a certain percentage of misplacement of the screws because you don't have the benefit of the 3D visualization of the spine,” Nguyen said. “It is not uncommon, while infrequent, when you have to take a patient back to the O.R. to revise a screw that was not placed perfectly.

“Every revision is another surgical trauma to the patient and it slows down the recovery, but since I have used this technology, I have not had a surgery that we've had to take back to revise.”
The technology is currently used only for spinal surgeries. Nguyen said he expects it to become available other surgical procedures as it develops.
With xvision, Nguyen wears a headset through which he looks at the patient rather than looking away at a monitor that displays X-rays of the surgical area. The effect is as if he is looking directly at an exposed spine to determine where to place rods and screws.
The result is a less invasive, more efficient and more accurate procedure that increases the safety to both the patient and the surgical team.
“Sometimes the patient’s anatomy is distorted or is blurred by scar tissue,” Nguyen said. “You have to take a lot of X-rays to ensure that you're doing your instrumenting safely, and that increases potential radiation exposure to the patient's body, to your body and to the staff. This augmented reality system allows you to take one spin (a single X-ray) and from that one spin, you can do the whole surgery and that has huge benefits not just to me in terms of reducing radiation exposure, but also to the patient and to everybody else in the room because it's lowering the radiation exposure to the rest of the team.”
With that imagery loaded into the system, the surgeon, through the headgear, can virtually peer through tissue to locate the abnormality and view the procedure as it takes place without looking away.
The “traditional navigation" of spinal surgery, as described by Nguyen, is taking a pre-operative or an intraoperative CT scan that is run through computer software, resulting in an image projected onto monitors, which provides guidance for the placement of screws. That requires looking away at the monitor while hands are working on the patient.
“The traditional navigation creates a discrepancy in the line of sight. You’re doing surgery on a patient, but you're not looking at the patient because you're looking at the monitor in order to navigate,” Nguyen said. “It allows us the benefit of navigation to safely determine where you are working in the patient's spine, while at the same time maintaining that line of sight where you're looking at the patient.
“This surgery allows us to see through scar tissue, and in cases where the patient's anatomy is distorted or contorted or deformed, it allows us the benefit of the 3D representation of the spine in real time on the patient's body so that we know exactly where we're putting the screw and exactly where we're putting the instruments.”
The technology also allows surgeries to be performed that were previously considered too risky or a low probability of a positive outcome.
“Before this technology, there would be patients who we would have to tell it's too dangerous or too difficult to do their surgery due to the scar tissue, due to the degree of deformity, due to abnormal variants in the anatomy,” Nguyen said. “Now we can safely and effectively and efficiently do surgery on just about anybody.”